Adult Healthy Weight

 Introduction
Introduction
Obesity is “one of the greatest long-term health challenges this country faces”1: a significant population health concern which results in long-term negative social, psychological and physical consequences.
The World Health Organization describes overweight as a condition of excessive fat deposits and obesity as a chronic complex disease defined by excessive fat deposits that can impair health2.
The diagnosis of overweight and obesity in adults is through measuring people’s weight and height by calculating the body mass index (BMI): weight (kg)/height² (m²).
For most adults, if your BMI is:
- Below 18.5 – you’re in the underweight range.
- 18.5 to 24.9 – you’re in the healthy weight range.
- 25 to 29.9 – you’re in the overweight range.
- 30 to 39.9 – you’re in the obese range.
- 40 or above – you’re in the severely obese range.
If you have an Asian, Chinese, Middle Eastern, Black African or African-Caribbean family background you’ll need to use a lower BMI score to measure overweight and obesity:
- 23 to 27.4 – you’re in the overweight range.
- 27.5 or above – you’re in the obese ranges3.
There isn’t a single intervention that can tackle obesity on its own, at population or at an individual level. Causes of obesity are multi-factorial, including biological; physiological; psycho-social; behavioural; and environmental factors.
 Why is it important to Population Health?
Why is it important to Population Health?
A healthy weight is a large contributor to overall health and quality of life. The effects of adverse body weight (underweight and excess weight) extend beyond physical health and can also have a bearing on mental wellbeing. Adverse body weight may influence an individual’s productivity and ability to undertake everyday tasks.
In the UK obesity is the second most common preventable cause of death after smoking.4
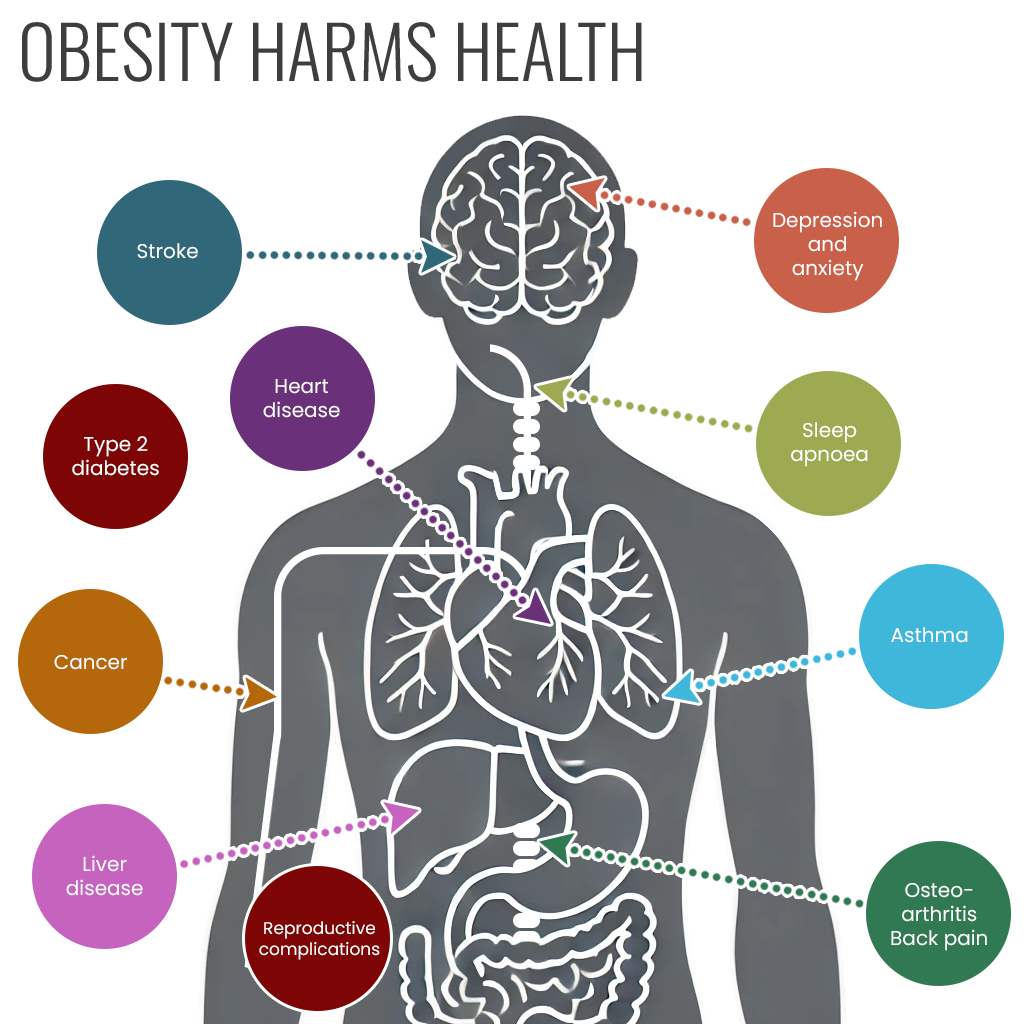
Overweight and obesity is associated with reduced life expectancy and is a risk factor of chronic diseases including cardiovascular disease, type 2 diabetes, at least 12 kinds of cancer, liver and respiratory disease, and obesity can negatively impact mental health.5
Obesity can also be associated with poor psychological and emotional health, and poor sleep. Obese adults may also be more likely to suffer from weight stigma which may impact on their self-esteem.6
Obesity can be detrimental and affects overall society and can have economic impacts, for example by affecting a person’s ability to work. Obese people are less likely to be employed, have more difficulty in re-entering the labour market, and when in work earn on average about 10% less than non-obese people. Overall, it is estimated that the indirect cost of obesity to the UK economy are £27 billion.7
Being underweight affects far fewer people than excess weight, both nationally and locally, but is also linked to increased risk of ill-health.
 The Derbyshire Population Health Approach
The Derbyshire Population Health Approach
The Derbyshire Population Health Approach focuses on prevention, population health, evidence-informed practices, causes, and collaboration. It emphasises proactive measures to prevent health issues, tailors interventions to specific populations, incorporates evidence-informed practices, addresses underlying causes, and promotes collaboration for effective action.
When considering the topic of adult healthy weight within The Derbyshire Population Health Approach:
• Prevention
Overweight and obesity is a notoriously difficult condition to reverse once established; four out of five children who are obese go on to become obese adults and many adults struggle to lose excess weight, often regaining any weight lost through dieting. Prevention therefore seems the best approach.
Prevention strategies for overweight and obese in adults in Derbyshire focuses on providing support, help and advice to achieve a healthy weight. Live Life Better Derbyshire provides a broader approach to weight loss than focussing on dieting, by providing a personalised approach that looks at emotional and psychological elements of weight management.
• Population
Some population groups are more at risk of developing overweight or obesity (and therefore the associated complications) than others.
These include:
- Those who are less well-off / experiencing social disadvantage.
- Older age groups
- People with disabilities
- Some black and minority ethnic groups
- Mental health (closely linked with obesity, can be affected by and affect each other)
- Children from families where at least 1 parent is living with obesity.
A compassionate communities’ approach will be taken, which will shift the blame away from individuals and fully acknowledges the impact of the conditions of people’s lives on their weight and health.
There will be a person - centred approach to tackling and addressing healthy weight is a priority. Targeting interventions to support communities who experience high levels of overweight and obesity are being developed and implemented to support specific needs of those communities.
• Evidence
We have a good understanding of the evidence around healthy weight in Derbyshire.
We will use evidence and insight to:
- Develop a deeper understanding of people and neighbourhoods experiencing greatest inequality.
- Listen to different perspectives and engage with people who have lived experience of inactivity.
- Share our collective insight and understanding to inform our work and the decisions we make.
- Develop and write a Food Plan for Derbyshire.
We will create opportunities and develop a whole system approach to develop a locality- based approach, working in collaboration with a wide range of partners and stakeholders.
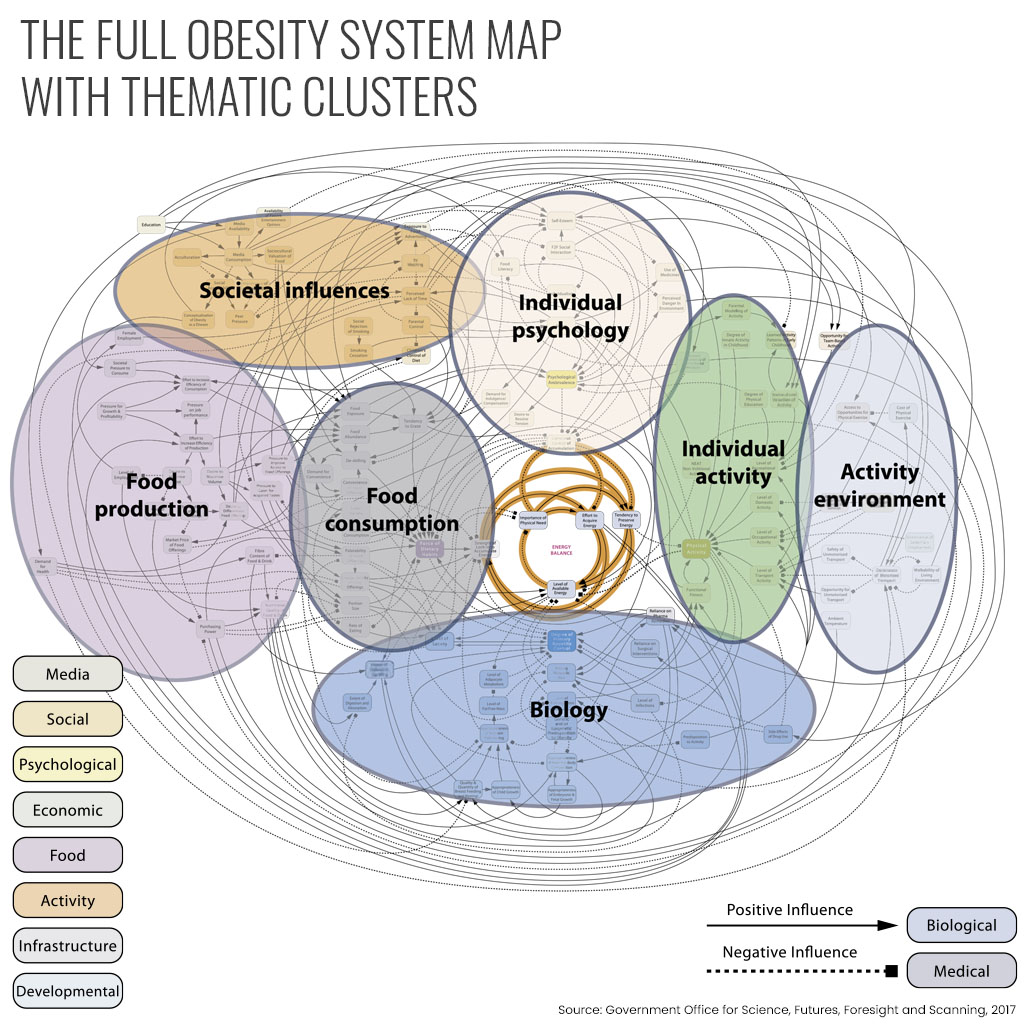
• Causes
Overweight and obesity result from an imbalance of energy intake (diet) and energy expenditure (physical activity).8 However this is a simplistic definition as it is a complex problem with a wide range of influences. A person’s body weight is subject to a complex interplay of biological, psychological, environmental, and economic factors. These include (but are not limited to):
- Universal factors (global food economy, governmental policies, multinational corporations),
- Local factors (food economy, health and education systems, socioeconomic status, affordability, access),
- Community factors (support systems, built environment, culture, beliefs, social networks), • individual factors (stress, cooking literacy, mobility, physical activity, mental health, life experiences/trauma)
- Intrinsic factors (genes, hormones, psychology).
Considering the breadth and inter-relationship of factors involved, tackling the wider determinants is a significant challenge which requires multi-agency collaboration. The Foresight system map below (Figure 1) shows the complexity of weight status and the number of factors that interact together.
• Collaboration
Collaboration is essential to addressing healthy weight. The development of a sustained ‘whole systems approach’ – health in all policies, actions across individual, environmental and societal levels involving multiple sectors (including planning, housing, transport, children’s and adult’s services, business and health) is required to improve adult healthy weight and obesity levels.
By incorporating healthy and sustainable food policy into the population health approach model, population health practitioners can implement targeted prevention strategies, address the underlying causes of overweight and obese, and foster collaboration to improve healthy weight and promote healthier communities.
In Derbyshire there are a range of interventions to support adults achieve a healthy weight.
Tier 2 – Live Life Better Derbyshire Adult weight management and lifestyle service
Live Life Better Derbyshire supports adult to achieve a healthy weight by delivering an adult weight management programme as part of an integrated lifestyle service.
Tier 3 – Specialist weight management
A multi disiplinary team, including physchologists, physicians, dieticians and weight loss advisors provide a personsliased service for people who are motivated to change and have attended tier 2 weight loss services.
Tier 4 – Bariatric Surgery
Offers an MDT assessment for bariatric surgery to patients who have successfully completed a Tier 3 weight management programme. The MDT includes dietitians, nurses, physiotherapists, psychologists, anaesthetists physicians and surgeons. Weight management / behavioural and lifestyle changes / optimising nutritional status before and after bariatric surgery.