Antimicrobial Resistance

 Introduction
Introduction
Antimicrobial resistance (AMR) arises when the organisms that cause infection find ways to survive treatment. Antimicrobials are medicines that treat infections. Examples, include antibiotics, antifungals and antiviral medication. Once standard treatments are ineffective, it is easier for infections to persist and spread.AMR causes people to suffer longer illnesses as infections become more difficult and in some cases, impossible to treat.
HM Government has placed AMR as a risk on the Civil Contingencies National Risk Register.1 The register outlines the most serious risks that the UK faces. It is listed alongside climate change as a chronic risk which can make other risks worse. There are a variety of actions individuals, organisations and communities can take to reduce the risk of AMR developing. There is a second national action plan and a 20-year vision to support the collaborative work to contain and control the impacts of AMR. Everyone in Derbyshire can make a difference.
 Why is it important to Population Health?
Why is it important to Population Health?
In the United Kingdom in 2019, there were 7,600 deaths attributable to AMR and 35,200 deaths associated with AMR. It threatens the core of modern medical practices, from the treatment of simple infections to more complex procedures like surgeries and cancer chemotherapy. As microbes become resistant to treatment, the risk of prolonged illnesses, increased healthcare costs, and mortality rises. This places substantial burdens on the health system in Derbyshire. It will also result in economic pressures on business and individuals through lost productivity and increased absenteeism.2
Health inequalities are avoidable differences in health between different groups of people. We know that there are differences in the number of antimicrobial resistant infections in different populations. There is ongoing work to identify whether these differences are avoidable.
According to the Organisation for Economic Co-Operation and Development (OECD) without sufficient action the costs to the UK associated with treating resistant infections could compare to having a COVID-19 pandemic every 5 years. AMR also impacts global health, food sustainability and security, environmental wellbeing, and socio-economic development. Effective antimicrobials are considered to be essential infrastructure for a functioning society.3
 The Derbyshire Population Health Approach
The Derbyshire Population Health Approach
The Derbyshire Population Health Approach focuses on prevention, population health, evidence-informed practices, causes, and collaboration. It emphasises proactive measures to prevent health issues, tailors interventions to specific populations, incorporates evidence-informed practices, addresses underlying causes, and promotes collaboration for effective action.
When considering the topic of AMR within The Derbyshire Population Health Approach:
• Prevention
AMR is a natural process as germs evolve to try and survive treatments such as antibiotics. This means that AMR cannot be entirely prevented. Every time an antimicrobial is used to treat an infection there is a risk of AMR. Misuse and overuse of antimicrobials are some of the key drivers in AMR, therefore reducing the need for antimicrobials by preventing infections and optimising their use are key priorities.
Initiatives to encouraging the uptake of vaccines are important as they help to reduce the burden of infections in the community. This reduces the need for antimicrobials. Vaccines reduce the burden of infectious disease by preventing the spread of it and reducing the severity of illness from infection. Other initiatives to strengthen the prevention of infection are promoting good respiratory and hand hygiene messages to reduce the burden of infection in the community. Additionally, strengthening infection, prevention and control measures in health and social care and agricultural sectors is vital.
Other population health initiatives focussed on raising community awareness regarding the risks of overuse and misuse of the medicines to treat infections are also used. Individuals can make a big difference in antimicrobial resistance by taking antimicrobials as directed by the prescriber, whether it’s for themselves, a family member or a family pet for example.
Good antimicrobial stewardship by health care professionals and in agriculture is also necessary to prevent AMR. Programmes to embed best practice in healthcare prescribing and audits are be used to protect antimicrobials. Encouraging safe disposal of any unused antibiotics is also key to reducing AMR and the impact on the environment.
Nationally and internationally, there are plans to support the research and design of new antimicrobials, however resistance can develop quickly. There have been no new classes of antibiotics since the 1980’s. Prevention of the progression of AMR in the first instance, is one of the key ways to protect the nation including the population of Derbyshire.
• Population
Data regarding AMR across some Health Inclusion Groups are limited though information on ethnicity and deprivation is available. Work continues nationally to understand differences in the use of antibiotics, and the impacts of AMR on populations.
There is strong evidence however that certain populations are at increased risk from infection and therefore likely to be more impacted by AMR. They include: the elderly, the very young, pregnant women, those who are immunocompromised. The population of Derbyshire is ageing this means that the impact of AMR will likely have a greater effect. The population profile for each district is varying, therefore even within Derbyshire the impacts of AMR will be felt differently.
The impact of AMR is unequal for certain populations, including those living with deprivation. Those experiencing higher levels of deprivation experience greater rate of infections, as well as increased resistance levels to antibiotics. The data also suggests differences between ethnic populations.
Carbapenemase-producing Gram-negative bacteria are an important marker of growing AMR In England. In 2022 the highest rate of this bacteria was noted in the Asian/ Asian British population. The rate was almost double that of the White population. Although the data suggests differences in terms of deprivation and ethnicity, more work is required to understand the reasons for those differences to work towards addressing health inequalities.4
The rate of AMR burden from blood stream infection and carbapenemase- producing gram negative bacteria notification per 100,000 population by index of multiple deprivation in 2022
Rolling quarterly average of E.coli blood specimens resistant to any one of the key microbials data is useful as a guide to overall trends of antibiotic resistance (lower percentage of resistance being better).
• Evidence
Surveillance systems are key in understanding the burden of AMR. There are global, national, and local systems to understand the number and type of antimicrobial resistant infections to assess the current risk to Derbyshire.
There is national evidenced based guidance available which is mandatory to follow for all NHS settings or settings where NHS services are delivered to prevent and control infections. The principles should be applied in all care settings.
Interventions to support antimicrobial stewardship are evidence based. Antimicrobial stewardship programmes developed by the UKHSA have been adopted locally. Campaigns such as Keep Antibiotics Working aim to reduce the expectation of receiving an antibiotic for a cold for example.
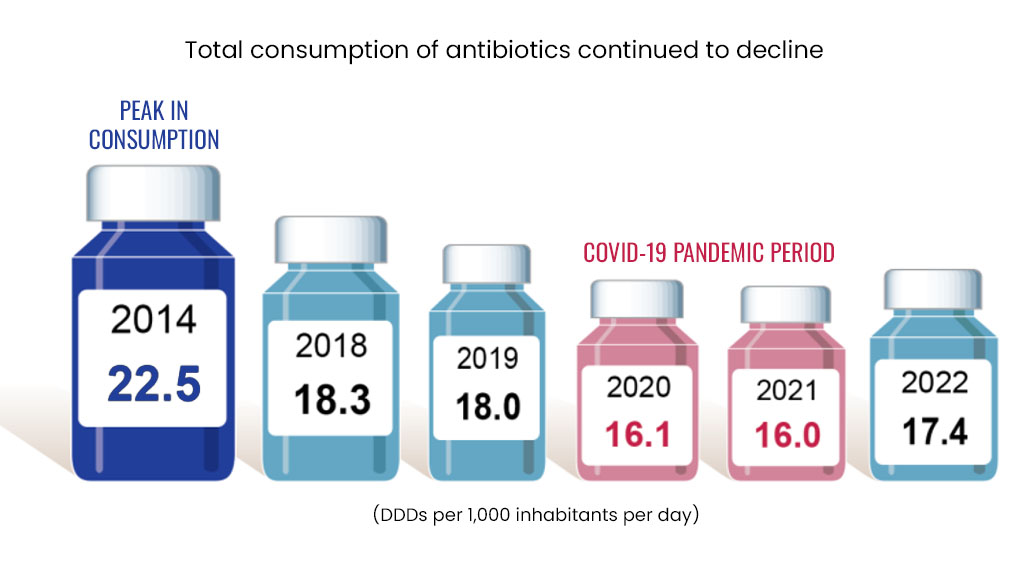
The use and overuse of antimicrobials, in particular antibiotics, are important factors for increasing AMR. There are measures to both monitor and control the use of antibiotics in England. These measures have led to a significant decline in antibiotic use since 2014.
Total consumption of antibiotics DDD per 1,000 inhabitants per day.5
• Causes
AMR is a natural phenomenon as germs rapidly evolve to protect themselves from antimicrobials. It cannot be entirely prevented however some actions can make it much worse. Every time an antimicrobial is used there is a risk of the germ becoming resistant to it. Misusing antimicrobials can increase the risk of it. One example of this is not completing the full course as directed by the prescriber or an antibiotic being given for a viral infection.
Other actions that increase the risk of AMR include the overuse of some pesticides and heavy metals. Antimicrobial resistance can spread from humans to animals and the environment. It’s important for all therefore that infections are prevented in animals and antimicrobials are used and disposed of responsibly.
There is also evidence that climate change could worsen the impacts of AMR. The climate is an important determinant of how infections behave and could have an impact on the populations at risk.
• Collaboration
Managing AMR effectively requires cooperation across multiple sectors including the general public. Everyone can do something to prevent AMR. Engaging healthcare providers, veterinarians, farmers, policymakers, and the community ensures that strategies are comprehensive and aligned with global efforts to tackle AMR. There is a Joined Up Care Derbyshire approach to enable an effective collaborative response.
 Latest Derbyshire Data
Latest Derbyshire Data
Trend Data
Prevalence Maps of Derbyshire
The maps below illustrate various geographies for Derbyshire. LSOAs and MSOAs are geographical divisions used for statistical purposes, allowing for more detailed analysis of local data. In these maps, you can explore various health indicators and data for Derbyshire, providing valuable insights into the area’s health and wellbeing.
 |
In the top right of the map, you’ll find the ‘Layer Control’ icon. This is an easy way to customise what you see on the map visualisation. Click the ‘Layer Control’ to choose which information is displayed on the map. Pick the indicator that interests you the most, and the map will transform accordingly. |
Slope Index
This chart illustrates the differences in health and lifestyle factors across areas in Derbyshire, from the most deprived (decile 1, red) to the least deprived (decile 10, green). As you move from left to right on the chart (from more deprived to less deprived areas), the line shows whether these factors are becoming more or less common. Essentially, it’s a way to see how living in wealthier or poorer areas affects the prevalence of these factors.
 Further Analysis & Assessments
Further Analysis & Assessments
Derbyshire Joint Strategic Needs Assessment (JSNA) involves a thorough examination of a specific health problem, exploring its causes, consequences, and underlying factors. It combines various data sources, collaboration with stakeholders, and rigorous analysis to generate insights for evidence-informed interventions and policy changes.
 More Information & Resources
More Information & Resources
Please speak to a healthcare professional if you are concerned about AMR. For further information, here is a list of useful resources about AMR. These materials are meant to provide individuals, healthcare professionals, and communities with the knowledge and tools they need as part of efforts to address AMR as a population health topic.
Contributors
Lauren Worrall, Advanced Ph Practitioner, Health Protection
Vijay Rai, Senior Pharmacist, NHS Derby and Derbyshire Integrated Care Board
Marie Hippey, Health Protection Officer, Health Protection